A comparison of Mepilex and conventional dressings
Patients with chronic wounds who were treated with atraumatic dressings such as Mepilex®, reported less pain and stress at dressing change than patients who received conventional dressings.
The impact of atraumatic vs conventional dressings on pain and stress
Upton, D., Solowiej, K. Journal of Wound Care 2012;21(5):209-215
- Wound pain can contribute significantly to stress and a variety of studies of biopsy, surgical and chronic wounds have shown that pain-induced stress can result in delayed wound healing.
- In addition to pain from the wound itself, pain can also result from continuous wound treatment, as well as anticipatory pain.
- Pain caused by the removal and re-application of dressings has been identified as a major contributor to wound pain.
- Patients may benefit from the use of atraumatic dressings as opposed to conventional dressings, since pain-induced stress has been shown to reduce healing rates of chronic wounds.
- Hence, appropriate dressing selection should form a significant part of recommended individual pain management plans.
- Atraumatic dressings, such as soft silicone, utilise technologies that have been developed to avoid adherence to the wound bed.
- It has been hypothesized that patients using atraumatic dressings as part of their treatment regimen might experience less pain at dressing change compared with when using conventional dressings.
Aims
To explore whether different dressing types were associated with the pain and stress experiences of patients with chronic wounds.
Methods
- This exploratory study was conducted to identify any differences between reported levels of pain and stress associated with the use of atraumatic and conventional dressings used in the treatment of patients with chronic wounds.
- The following psychological measures were implemented:
- The Perceived Stress Scale (PSS)
- The State Trait Anxiety Inventory (STAI)
- A numerical stress rating scale
- At dressing change, the PSS and STAI questionnaires were read aloud to each patient and verbal responses were recorded by a member of the research team.
Results
- Of 49 patients with chronic wounds, 53% were male (n=26) and 47% were female (n=23). Age ranged between 38 and 95 years, with a mean age of 69.1±14.1.
- Wound types were of varying aetiologies and were treated with either atraumatic dressings, such as Mepilex, or conventional dressings such as Biatain®* or Aquacel®* Ag, (Table 1).
*Aquacel is a registered trademark of ConvaTec Inc. Biatain is a registered trademark of Coloplast A/S.
Table 1. Wound aetiology
| Wound type | Atraumatic n(%) | Conventional n(%) |
| Venous leg ulcer | 3 (30%) | 5 (13%) |
| Other leg ulcer | 2 (20%) | 5 (13%) |
| Diabetic foot ulcer | 1 (10%) | 15 (38%) |
| Other foot ulcer | 4 (40%) | 8 (21%) |
| Other chronic wound | - | 6 (15%) |
| Total | 10 | 39 |
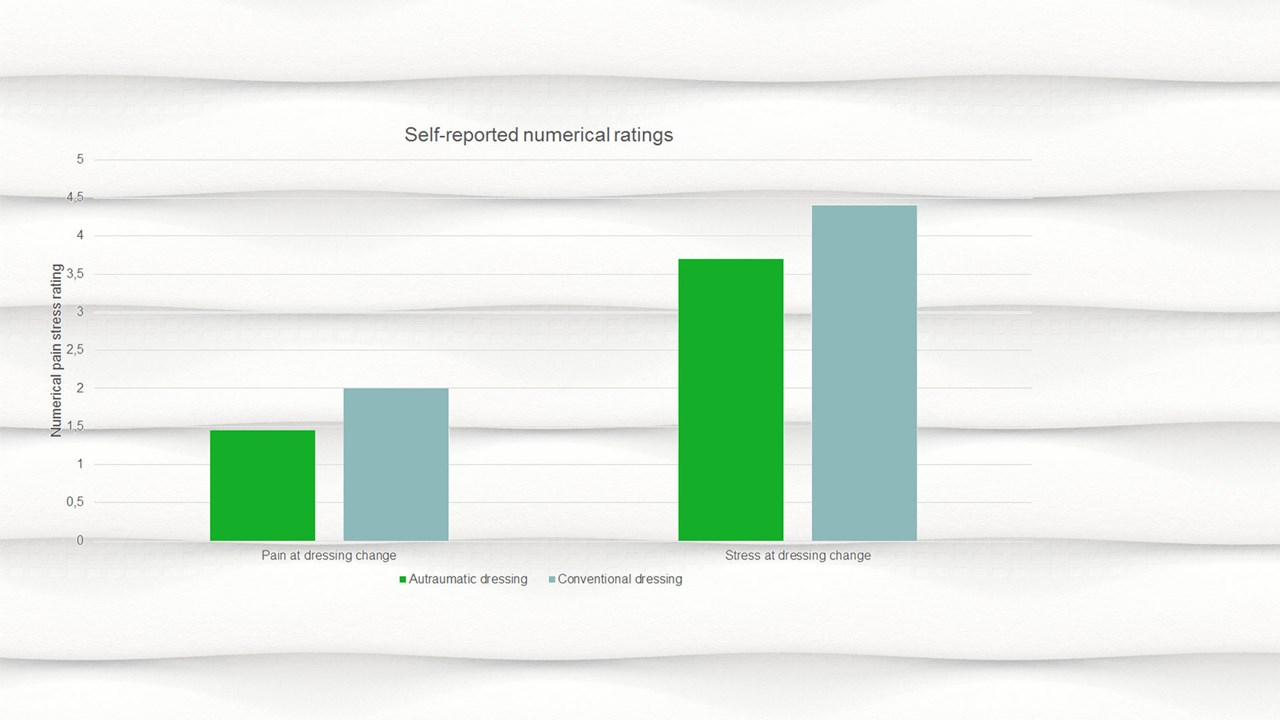
- Patients treated with conventional dressings experienced significantly higher numerical pain ratings (p is less 0.05), numerical stress ratings (p is less than 0.05), and (GSR less than 0.05) at dressing change, compared with the atraumatic dressing group.
- Although the differences in physiological measures were non-significant, the mean heart rate (75.62±14.05), systolic BP (137.82±17.03), diastolic BP (69.13±12.91) and salivary cortisol (0.17±0.09) scores were higher in the conventional dressing categories than for the atraumatic categories (Table 2).
Table 2. Mean psychological and physiological pain and stress scores for patients receiving atraumatic and conventional dressings
| Pain/stress measures | Atraumatic | Conventional |
| STAI | 38.40 ± 15.62 | 33.1 ± 11.16 |
| PSS | 24.60 ± 10.08 | 22.72 ± 9.17 |
| Numerical pain | 1.43 ± 0.98* | 3.66 ± 3.13* |
| Numerical stress | 2.00 ± 0.58* | 3.63 ± 2.66* |
| Heart rate | 69.11 ± 7.53 | 75.62 ± 14.05 |
| Respiration rate | 16.86 ± 8.17 | 16.09 ± 1.95 |
| Systolic blood pressure (BP) | 125.70 ± 12.23 | 137.82 ± 17.03 |
| Diastolic blood pressure (BP) | 64.22 ± 11.56 | 69.13 ± 12.91 |
| Galvanic skin response (GSR) | 19.76 ± 5.42* | 33.15 ± 16.32 |
| Salivary sortisol | 0.13 ± 0.03 | 0.17 ± 0.09 |
*Difference between groups statistically significant at p less than 0.05
STAI = state trait anxiety inventory; PSS = perceived stress scale
- In addition to the increased physiological indicators of stress among patients receiving conventional dressings, the self-reported severity of acute pain and stress also demonstrated higher pain and stress at dressing change for the conventional dressing group (Figure 1).
- Stress scores on the PSS and STAI were relatively similar for patients receiving both types of dressings. Mean PSS scores were 24.60±10.08 for patients receiving atraumatic dressings and 22.72±9.17 for patients with conventional dressings, out of a maximum PSS score of 56.
- Patients with atraumatic dressings scored an average of 34.90±11.41 for underlying anxiety and 38.40±15.62 for acute anxiety at dressing change, in comparison with the conventional dressing group, who scored an average of 33.21±11.20 for trait anxiety and 33.31±11.16 for acute anxiety at dressing change on the STAI, out of a maximum score of 80.
- Patients’ average levels of underlying stress were 24.60 ± 10.08 (atraumatic dressings group) and 22.72 ± 9.17 (conventional dressings group) on the PSS and 34.90 (atraumatic dressings group) and 33.21 (conventional dressings group) on the STAI.
- This could be taken to suggest that, although acute episodes of pain and stress were much lower in patients receiving atraumatic dressings, factors associated with the overall experience of living with a chronic wound may be contributing to underlying and ongoing feelings of stress and anxiety.
Conclusion
- Patients receiving atraumatic dressing as part of their wound treatment experienced significantly lower self-reported episodes of acute pain and stress at dressing change compared with patients being treated with conventional dressings.
- The atraumatic dressing group had reduced physiological signs of acute stress in comparison with the conventional dressings group, including lower heart rate, systolic and diastolic BP, GSR, and salivary cortisol at dressing change.
- Overall, the results of this study support the notion that appropriate selection of dressings can contribute to a reduction in acute pain and stress, which could lead to an overall improvement in wound treatment experience. These findings may also have implications for the cost of wound care.






